Many times the family is unaware that they have this disease myotonic dystrophy in their families. The birth of an infant with CMD is the first time this disease is diagnosed or what in the medical area is know as the index case. Others know they have the DM1 disease but are unaware of the more severe congenital form. Congenital Myotonic Dystrophy is difficult because of the birth of an infant with issues with the disease. It is also difficult because the mother is affected. Over time the mothers symptoms will get progressively worse as well.
 Hypotonia: This is defined as weakness and floppiness of the muscles. The infant will demonstrate what is known as low tone. This is one of the most prominent features of CMD. It is generally the cause of much immediate medical attention. In the more severe cases the Hypotonia is profound and may resemble that of a premature infant although most cases of CMD will have a normal birth weight and gestation.
Hypotonia: This is defined as weakness and floppiness of the muscles. The infant will demonstrate what is known as low tone. This is one of the most prominent features of CMD. It is generally the cause of much immediate medical attention. In the more severe cases the Hypotonia is profound and may resemble that of a premature infant although most cases of CMD will have a normal birth weight and gestation.
Hypotonia is often referred to as “floppy baby syndrome” because the child feels and looks like a rag doll in your hands.Most newborns will hold themselves rigid if held in the air by their torso alone, while a hypotonic baby will just droop.They are not able to maintain flexed ligaments, but they are able to extend ligaments beyond normal lengths.They also really cannot control the movements of their heads, making them even more likely to flop their heads around than a healthy newborn. It’s important to hold a hypotonic baby carefully, because they will not resist at all.If you’re not careful, they can just slip right through your hands and arms. Never try to hold a hypotonic baby under their arms, they’ll fall right through. Instead, support them firmly with your hands on their torso.
With CMD the infant will make steady improvement and the Hypotonia will in most cases disappear by age 3-4. In many cases the hypotonia might be mistaken for some cerebral disorders before it is realized that there is an underlying neuromuscular problem. This link by the medical profession to cerebral disorders may involve doctors giving the infant a poor outlook; Such as the infant “may never walk” It is quite surprising to many parents and doctors and the infants and toddlers make progression. Once CMD is diagnosed then, more sense will come as to this progress. Reflexes: Besides the low tone there may be a diminished Cry and Suck Reflex. The diminished suck reflex may be due to the low tone above
 Polyhydraminos: Many mothers of CMD will have excess fluid before birth. This excess fluid may cause premature labor. Amniotic Fluid which surrounds the baby is generally swallowed by the infant and excreted through the babies kidneys. Because of the lack of suck reflex the infant does not swallow and excrete the fluid. The mother continue to produce new fluid and thus fluid builds up in the mother. This build up of fluid may or will cause premature labor.
Polyhydraminos: Many mothers of CMD will have excess fluid before birth. This excess fluid may cause premature labor. Amniotic Fluid which surrounds the baby is generally swallowed by the infant and excreted through the babies kidneys. Because of the lack of suck reflex the infant does not swallow and excrete the fluid. The mother continue to produce new fluid and thus fluid builds up in the mother. This build up of fluid may or will cause premature labor.
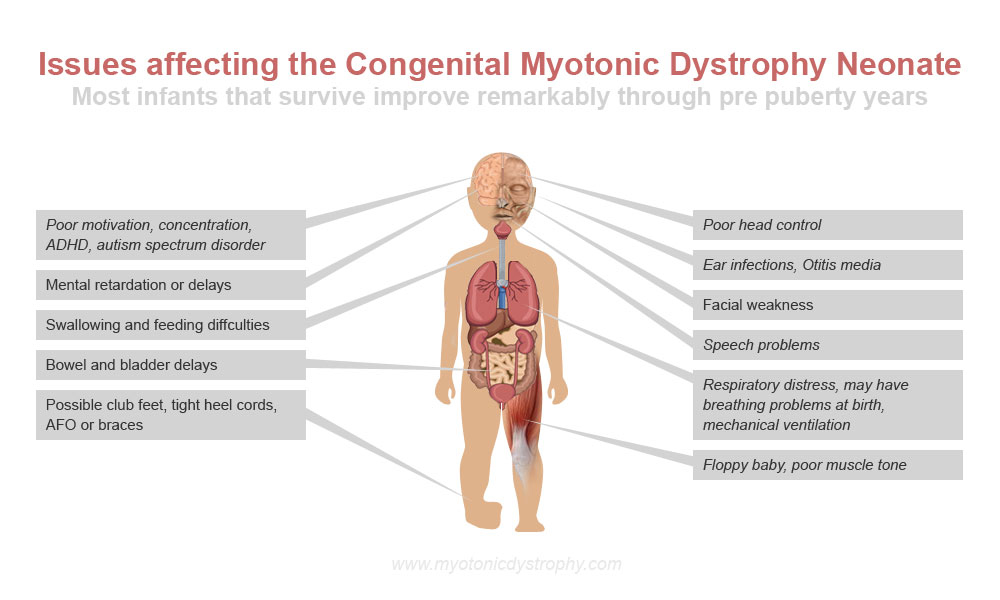
 Respiratory Distress: Many infants have breathing problems when born. Four reasons may exist for this problem
Respiratory Distress: Many infants have breathing problems when born. Four reasons may exist for this problem
1. Diaphragmatic and intercostal muscle involvement
2. Pulmonary Immaturity
3. Aspiration pneumonia
4. Failure of Cerebral Respiratory control
Previous to the modern availability of medical support such as mechanical ventilators many CMD infants would die as the respiratory function was insufficient to sustain life. With modern support many of these infants will survive. Rutherford in a review stated that of 14 severely affected neonates all those requiring ventilation for more than 4 weeks died from respiratory problems. However other studies dispute this. Infants not needing mechanical ventilation may still have problems with cyanosis and Apnea. Problems with breathing may be heightened during the feeding process. Care must be taken not to have the infant aspirate food when they are eating. Respiratory problems will rarely persist past the first month of life. Note: There have been cases of babies on ventilators for over 60 days that have recovered.
 Malformations: The hypotonia may result in malformations as the infant inside the mother is unable to resist the positional forces in the Uterus.
Malformations: The hypotonia may result in malformations as the infant inside the mother is unable to resist the positional forces in the Uterus.
Thin Ribs: Infants with CMD will on X-Ray show thin ribs.
Clubfoot: This is also the frequent result of CMD. Technically this will be know as Talipes. About 50% of cases studied by Harper had Talipes. at birth. This was a contributing factor in delay of motor develop for these children. Most of the cases of talipes are bilateral or present on both sides of body. Treatment for this would be active surgical correction as most children with CMD will be able to walk
and be mobile as there is a steady progression of motor function in early childhood The mean walking age of children with Talipes was 29.1 months. Without Talipes the mean age for walking was 23.4. The average walking age for both groups was 27.1 (Reardon out of 61 cases)
 Adolescent Onset: In all or most CMD instances the CMD will develop the standard myotonic dystrophy in the late teens or early 20’s. Muscle weakness will occur in facial muscles and extremities. This is a unique dual nature of the congenital form of myotonic dystrophy. In fact, congenital form is in many ways distinct from the adult form with separate symptoms see chart above and then a separate set of symptoms see the section on general information on myotonic dystrophy
Adolescent Onset: In all or most CMD instances the CMD will develop the standard myotonic dystrophy in the late teens or early 20’s. Muscle weakness will occur in facial muscles and extremities. This is a unique dual nature of the congenital form of myotonic dystrophy. In fact, congenital form is in many ways distinct from the adult form with separate symptoms see chart above and then a separate set of symptoms see the section on general information on myotonic dystrophy
 Ear Infections: For a variety of Reasons Children with CMD are prone to ear infections and may need ear tubes and prophylactic antibiotics. This ear infections may interfere with hearing if not promptly treated. Because of the nature of CMD many CMD children will not or can not report if they have an ear infection. Aggressive treatment is recommended with frequent doctor visits, training of parents to detect ear infections, antibiotics, and ear tubes. Failure to contain the problem with ear infections may cause hearing problems .More information on Ear Infections
Ear Infections: For a variety of Reasons Children with CMD are prone to ear infections and may need ear tubes and prophylactic antibiotics. This ear infections may interfere with hearing if not promptly treated. Because of the nature of CMD many CMD children will not or can not report if they have an ear infection. Aggressive treatment is recommended with frequent doctor visits, training of parents to detect ear infections, antibiotics, and ear tubes. Failure to contain the problem with ear infections may cause hearing problems .More information on Ear Infections
 Braces: In many cases children will require AFO (Plastic Braces) to assist in walking and muscle problems in the Feet lower legs
Braces: In many cases children will require AFO (Plastic Braces) to assist in walking and muscle problems in the Feet lower legs
 Facial Weakness: On both sides of the face often severe in nature is weakness of the muscles. This is often the most easily visible feature of CMD. It can be easily observed and also will be noted by the inability to suck due to muscle weakness. For more information on this Click here. OralFacila Dysfunction in Children with Myotonic Dystrophy
Facial Weakness: On both sides of the face often severe in nature is weakness of the muscles. This is often the most easily visible feature of CMD. It can be easily observed and also will be noted by the inability to suck due to muscle weakness. For more information on this Click here. OralFacila Dysfunction in Children with Myotonic Dystrophy
Upper Lip: The upper lip of affected infants will resemble an inverted Letter “V” Below is a picture of a 6 year old showing this inverted “V”
Myotonia: It is very interesting to note that myotonia the cardinal feature of standard Myotonic Dystrophy is completely absent in CMD. If an infant shows signs of myotonia then a different diagnosis should be suspect such as myotonia congenita or Schwartz-Jampel Syndrome. Clinical myotonia will develop with age:
Less than one year old 0% affected
Age 1-5 years 12%
Age 6-10 Years 75%
11 years Plus 100%
Information from Harper on all types of CMD Based on over 100 cases
Facial Weakness 85.7%
Hypotonia 69.8
Delayed Motor Dev 64.3
Mental Retardation 62.7
Talipes (Clubfoot) 52.4
Respiratory Distress 47.6
Feeding Problems 57.1
Hydraminos 25.4
Reduce Movement 22.2
From Fetus
Muscle Strength in all Types of CMD
Muscle strength in most patients improved up to 5 years in age since motor development surpassed disease progression. From ages 5-20 patients remained stationary or showed slowly progressive decline. After age 20 years, all patients gradually worsened. (Kobayashi)
Generally these cardiac problems are not present in the early years of the congenital and some juvenile forms of.Myotonic Dystrophy. Make sure your doctor is aware of this issue. A major concern for all patients with either CMD or Myotonic Dystrophy is cardiac problems. About 11% of patients in one study died suddenly from Heart Problems. Please make sure to visit the special section on Cardiac problemsfor more information. There is preventative steps that can be taken.
Symptoms: Mothers may exhibit more or more of the following in a variety of severity’s
- Polyhydraminos (Excess amniotic fluid during pregnancy)
- Constipation
- Ulcerative Colitis
- Hair Loss
- Depression
- Apathy/Lack of Motivation
- Difficulty in swallowing
- Abnormal ECG
- Weakness in muscles
- Inability to rapidly open and close hand
- Hypersomnia (Excessive sleeping)
Because of these facts that some mothers have Myotonic Dystrophy they may have a difficult time caring for their children. Its very important to have an active management program by an unaffected family member to help the mother manage her symptoms.
Video on Congenital Myotonic Dystrophy
Click here to see a video by MDF on a mom and toddler that has myotonic dystrophy. This is good basic information on what is involved in helping a youngster with myotonic dystrophy.
Click here to see another video by MDF on Congenital Myotonic Dystrophy. This is a lecture by Dr. Sampson who is well known in the field. This is more medical and has more in depth information.
 Treatment Right now all the treatments are just symptom based. (BREAKING NEWS SEE BELOW!!) There is no cure or final treatment for myotonic Dystrophy. However, the researchers now know what causes the disease and that is a triplet expansion. There are drugs in development such as the one by Isis pharmaceuticals in Carlsbad, CA. The drug has had great success when tried on Rodents that had myotonic dystrophy. The drug still needs more testing and will be 5-8 years away still. Its unknown if the drug can cure all the symptoms of the congenital form of myotonic dystrophy such as IQ decrease. The treatment though worked very well, one injection kept the disease away from the rodents for months. It is hopeful but not guaranteed as humans are more complex than rodents. Hundreds of researchers are working now on a cure for this disease, all over the work. The next major meeting or researchers is in 2015 in Paris. IDMC-10
Treatment Right now all the treatments are just symptom based. (BREAKING NEWS SEE BELOW!!) There is no cure or final treatment for myotonic Dystrophy. However, the researchers now know what causes the disease and that is a triplet expansion. There are drugs in development such as the one by Isis pharmaceuticals in Carlsbad, CA. The drug has had great success when tried on Rodents that had myotonic dystrophy. The drug still needs more testing and will be 5-8 years away still. Its unknown if the drug can cure all the symptoms of the congenital form of myotonic dystrophy such as IQ decrease. The treatment though worked very well, one injection kept the disease away from the rodents for months. It is hopeful but not guaranteed as humans are more complex than rodents. Hundreds of researchers are working now on a cure for this disease, all over the work. The next major meeting or researchers is in 2015 in Paris. IDMC-10
BREAKING NEWS ON TREATMENTS: A recent study (Dec 2015) by Japanese and Polish researchers have found that Erythromycin an FDA approved drug might help with the treatment of Myotonic Dystrophy. This drug helped with the treatment of gastric symptoms in patients with myotonic dystrophy in a separate study in 2002. As the Congenital form of the disease is more severe and affects the brain more your doctor may want to consider this treatment. Read more about this potential treatment here.
The William Singeris National Center for Myotonic Dystrophy in Canada
The William Singeris National Centre for Myotonic Dystrophy was officially opened Monday December 20 2004 with a commitment of $ 237,700.00 over five years by Phil and Megan Singeris and their family of supporters. Inspired by their 2 year old son William who has Congenital Myotonic Dystrophy, Phil and Megan wanted to do something to help others suffering from this little known disease. A fundraising gala was held in April 2004 with the goal of raising $30,000.00. When the final results came in, the astonishing total of over $60,000.00 was realized! The Centre based in London at Children’s Hospital of Western Ontario and Children’s Health Research Institute will for the first time in Canada, document and track all children born in Canada with Myotonic Dystrophy and follow their development and treatments for five to ten years.This data will not only form a critical foundation for development and testing of treatments that could eventually lead to a cure, but will also provide much needed information to parents and prospective parents of children with this disease to help base family decisions on more solid facts. Led by Dr. Craig Cambell, Paediatrician at Children’s Hospital of Western Ontario and Associate Scientist, Children’s Health Research Institute, the research process has already begun. “Information and questionnaires will be sent to every paediatrician in Canada each month asking for reports on any child with Myotonic Dystrophy,” said Dr. Campbell. “In addition to medical information and annual development testing, we will look at quality of life measures for both the child and family. The Child Health and Well- being Program at Children’s Health Research Institute has one of the best known research groups in Canada to study such impact on children and their families”. Thank you to Phil, Megan, Stephanie and especially William Singeris for an amazing gift to children all over Canada!
Below is a link to a fact sheet on Congenital Myotonic Dystrophy from England
Congenital Myotonic Dystrophy Fact Sheet
Brochure from the MDSG support group England


I really enjoyed reading this article, it was very informative. My son Andrew was born in July of 2009 with Congenital Myotonic Dystrophy. I had polyhydraminos Andrew was born at my 35 week check up. Not one doctor ever suspected anything was wrong, I did often ask the doctor why Andrew never kicked me like the three other children I had given birth too. She told me it was because he was breech the entire time they tried to turn him however this caused my to dialate at my 35 week checkup to 7 cm. I think the pressure of the fluid played a big role in this. Andrew has had many surgeries, he had his Gtube and surgery a month after being born due to his inability to eat. He then had his heel and toe cords lengthened, then shortly after that surgery he had his tonsils and adniods removed because he had severe sleep apnea. He has been through a lot but I see big improvements as he gets older. He can now walk without his walker, he still will always have braces most likely, he also is eating just about anything by mouth. I still have to supplement via G-tube at night but not as much as we had too. I am concerned about his future especially the ADHD part he really has no attention span. I would like to know other families with older children that are school age to see how they do in school, and to know if they did develop heart issues as they age. Andrew has been to a heart doctor but they have no cause for concern at this time.