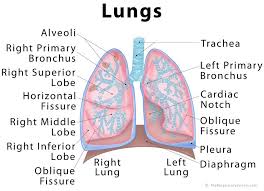
A new study of myotonic dystrophy patients indicates that an older style test of maximum voluntary ventilation may help Myotonic Dystrophy patients know their lung function better.
The maximal voluntary ventilation (MVV) is another measure of the neuromuscular and respiratory systems. The MVV is the total volume of air exhaled during 12 sec of rapid, deep breathing, which can be compared with a predicted MVV defined as the forced expiratory volume in 1 sec (FEV1) × 35 or 40. A significant difference between the predicted and measured MVV may indicate insufficient neuromuscular reserve, abnormal respiratory mechanics, or an inadequate effort. Progressive reduction of tidal volumes during the test is consistent with neuromuscular abnormalities but also occurs with gas trapping as a result of disorders that cause airflow limitation.
Clinical_implication_of_maximal_voluntary.-ventilation-in-Myotonic-Dystrophy