Cataracts
CATARACTS
Cataracts are a common problem with Myotonic dystrophy. Often it will be the first symptom of the disease. These are easy treatable with replacements often at a low-cost.
Cataract Brochure Myotonic Dystrophy (PDF)
Information on eyes and Dry eyes
| Yichieh Shiuey, MD and Theresa C. Chen, MD Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, MA |
 |
What type of cataract is this?
Answer: Christmas tree cataract.
What systemic medical condition is classically associated with these lens findings?
Answer: Myotonic dystrophy
What other ocular findings may this patient have?
Answer: Ptosis, orbicularis weakness, progressive external ophthalmoplegia, and pigmentary retinopathy similar to that of Kearn’s Sayre syndrome. Aside from Christmas tree cataracts which contain multicolored iridescent crystals, patients with myotonic dystrophy may also have spokelike cortical opacities along the suture line.
What general physical examination findings may this patient have?
Answer: Myotonia is the often the first detectable physical exam finding. This may be strikingly demonstrated by shaking hands with the patient. The patient may not be able to release his or her grip. Patients with myotonic dystrophy may also have weakness of the limb muscles, particularly the leg extensors. Atrophy of limb muscles may also be apparent on inspection. Men in this condition often have early onset of frontal baldness.
What is the inheritance pattern of this systemic medical condition?
Answer: autosomal dominant
| A Call for Cataract Samples |
| The early appearance of cataracts is an important feature of Myotonic Dystrophy and is often the only obvious symptom in those only mildly affected. This suggests that the lens of the eye is particularly sensitive to Myotonic Dystrophy making it an important target for research.The Norwich Eye Research Groupheaded by Professor George Duncan is one of the foremost centres for lens research in the world. The causes of cataract as well as the development of improved treatments are the central themes of our work. As a member of the group I am heading the Cataract in Myotonic Dystrophy Project.To carry out our research we would like to obtain tissue samples from people with Myotonic Dystrophy. During a normal cataract operation a small piece of tissue is removed from the front of the lens and discarded by the surgeon. At no inconvenience to the patient this small piece of tissue, can be preserved and would be sufficient for us to carry out some extremely valuable work. Not only will it help us to understand how Myotonic Dystrophy causes cataract in the lens but it could give us more fundamental information about the disease as a whole.
Without your support this type of research would not be possible. So can I ask that if you are considering having a cataract operation you contact us either directly here in Norwich (j.rhodes@uea.ac.uk) or via the Myotonic Dystrophy Foundation in Palo Alto , CA and we will arrange with your Ophthalmic consultant for collection of the samples. Thank you. Dr. Jeremy D. Rhodes. The Norwich Eye Group, School of Biological Sciences, University of East Anglia, Norwich, NR4 7TJ, UK |
Dental Needs
Dental Needs of Patients with DM
Because of the nature of Myotonic Dystrophy, patients need increased dental care. This can come in several forms but the decreased amount of muscle strength can affect the person with DM. They may have more plaque and need more frequnet brushing and dental hygiene. We have found a few articles and stories that focus on dental care that you may wish to review. Print out the first one and take it to your dentist.
Diabetes
DIABETES
This page will try and summarize information on myotonic dystrophy and diabetes.
Study:
Pathogenesis of Diabetics in Myotonic Dystrophy.
Myotonic dystrophy (MD) is the most common adult form of muscular dystrophy with an estimated prevalence of 1 in 8000 and is often complicated by diabetes. MD is dominantly inherited and is due to heterozygosity for a tri-nucleotide repeat expansion mutation in a protein kinase gene and it was suggested that this induces derangement of RNA metabolism also able to reduce insulin receptor expression. To test whether the abnormal RNA metabolism or a specific malfunction of protein kinase gene may induce insulin resistance prior to the onset of diabetes, we studied 5 glucose-tolerant MD patients (3F/2M, 41 [+ or -] 8yrs, 59 [+ or -] 7 kg, BMI21 [+ or -] 2 kg/[m.sup.2]) and 5 matched healthy subjects, by means of a) dual x-ray energy absorption b) euglycemic-hyperinsulinemic clamp (1 mU/kg/min) c) primed-continuous infusion of 6,6-[d.sup.2]-glucose and I-[sup.13]C-leucine d) indirect calorimetry. Fasting plasma insulin were similar, but proinsulin concentrations were increased in M!
D patients (p=0.01) and the ratio intact proinsulin/insulin (20 [+ or -] 4% vs 5 [+ or -] 1%; p=0.01) was 4-fold higher in MD. MD showed increased body fat mass (35 [+ or -] 5 vs 26 [+ or -] 2%; p=0.05) but lipid oxidation and FFA concentration in the post absorptive and clamp conditions were comparable between the two groups. Glucose metabolism (oxidative and non-oxidative) during insulin stimulation was comparable to normals (6.9 [+ or -] 1.4 vs 8.2 [+ or -] 1.1 mg/]kg FFM.min]; p=0.49). Leucine flux in the post absorptive condition was slightly increased and its sensitivity to insulin was impaired in MD (suppression =8[+ or -]2 vs 19 [+ or -] 2%; p=0.05); also suppression of plasma glutamine (8 [+ or -] 5%) and phenylalanine (8 [+ or -] 2%) concentrations during the clamp were similar than in normals (33 [+ or -] 7 and 15 [+ or] 3% respectively; p=0.05). In summary, MD showed alterations of protein metabolism in both post absorptive and insulin stimulated conditions resulti!
ng in increased proteolysis and muscle wasting. Insulin dependent glucose metabolism is preserved; therefore insulin resistance for glucose is not a major factor in the pathogenesis of diabetes in MD. On the contrary, abnormal insulin cleavage leading to increased proinsulin levels, probably related to specific protein kinase gene malfunction, represents a marker of secretory dysfunction capable to induce diabetes mellitus.
GIANLUCA PERSEGHIN, MAURO COMOLA, CINZIA ARCELLONI, EMANUELA PAGLIATO, ROBERTO LANZI, ALBERTO BATTEZZATI(*), LIVIO LUZI(*), Milan, Italy
(*) ADA Professional Section Member. See Duality of Interest Information.
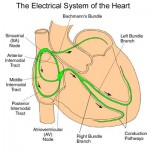
Heart and Myotonic Dystrophy
|
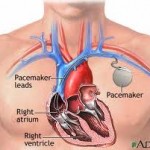
Conduction disturbance can lead to abnormal heart rhythms called arrhythmias. Arrhythmias that are too slow sometimes require a pacemaker that delivers regularly timed electrical impulses to bring the heart rate up to normal. When the heart rhythm is too fast, an implantable defibrillator can deliver an electrical shock to restore a normal heart rhythm. These are called ICD’s the underlying problem with the heart in myotonic dystrophy s fibrosis and abnormalities in the heart that seem to specifically and primarily affect the conduction system, the specialized tissue that allows for electricity to flow through the heart. It leads to a higher risk of arrhythmias, and a small percentage of patients develop cardiomyopathy.” The most serious arrhythmias are those that cause the lower chambers of the heart — the ventricles — to stop beating or to beat too slowly to sustain life; or to beat in a fast, uncoordinated and ineffective way. Both these fast and slow ventricular arrhythmias can lead to sudden death, and people with MMD1 unfortunately are at increased risk for that. Here is a great video from the Library at the Myotonic Dystrophy Foundation. This video talks about the heart and the electrical issues in the heart with Myotonic Dystrophy |
|
Pacemakers and Defibrillators: Pacemakers are generally used to manage a heartbeat that is too slow or irregular, caused by disorders that disrupt the heart’s normal electrical conduction system. This condition known as bradicardia can cause inadequate blood flow through the body creating symptoms such as fatigue, dizziness, and fainting.
|
CK Recommendations for Patients with DM from Scottish Workgroup
|
|
*This information was copied from the evidence based clinical guidelines developed by the Collaborative Project Byall Scottish Clinical Genetics Services.
|